Rectal Prolapse
Understanding Rectal Prolapse: Causes, Symptoms, and Effective Treatment Options by Dr. Yogendra Rai at Rai Piles Health Clinic
Rectal prolapse is a medical condition that, while not commonly discussed, can significantly impact a person’s quality of life. At Rai Piles Health Clinic, under the expert guidance of Dr. Yogendra Rai, we specialize in diagnosing and treating rectal prolapse and other anorectal conditions. In this comprehensive blog, we’ll explore everything you need to know about rectal prolapse, including its causes, symptoms, diagnosis, and the various treatment options available. By the end of this article, you’ll have a clear understanding of how Dr. Yogendra Rai and his team can help you manage and overcome this condition.
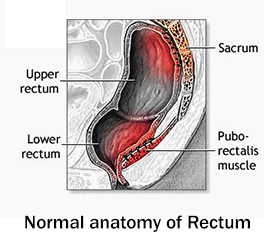
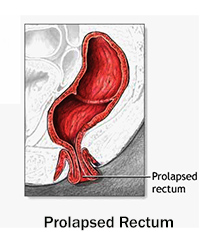
What is Rectal Prolapse?
Rectal prolapse occurs when the rectum (the lower part of the large intestine) slips out of its normal position and protrudes through the anus. This condition can be partial, where only the lining of the rectum protrudes, or complete, where the entire wall of the rectum extends outside the body. Rectal prolapse can cause significant discomfort, pain, and embarrassment, and it often requires medical intervention to correct.
Causes of Rectal Prolapse
Understanding the root causes of rectal prolapse is essential for effective treatment and prevention. Some of the most common causes include:
- Chronic Constipation:
Straining during bowel movements over a long period can weaken the muscles and ligaments that support the rectum, leading to prolapse. - Chronic Diarrhea:
Frequent bowel movements can also strain the rectal muscles and contribute to prolapse. - Aging:
The muscles and ligaments in the pelvic area can weaken with age, increasing the risk of rectal prolapse. - Childbirth:
The strain and pressure during childbirth, especially multiple vaginal deliveries, can weaken the pelvic floor muscles and lead to prolapse. - Pelvic Floor Dysfunction:
Weakness or dysfunction in the muscles and ligaments that support the pelvic organs can contribute to rectal prolapse. - Neurological Conditions:
Conditions like multiple sclerosis or spinal cord injuries can affect the nerves that control the rectal muscles, leading to prolapse. - Previous Surgery:
Surgery in the pelvic or anal area can sometimes result in weakened support structures, increasing the risk of prolapse. - Genetic Factors:
Some individuals may have a genetic predisposition to weaker connective tissues, making them more susceptible to rectal prolapse.
Symptoms of Rectal Prolapse
The symptoms of rectal prolapse can vary depending on the severity of the condition. Common signs and symptoms include:
- Protrusion of the Rectum:
The most obvious symptom is the protrusion of the rectum through the anus, especially during bowel movements. - Pain and Discomfort:
Pain in the rectal area, especially during bowel movements or sitting, is a common symptom. - Bleeding:
The protruding tissue may become irritated and bleed, leading to bright red blood on toilet paper or in the toilet bowl. - Mucous Discharge:
A mucous discharge from the anus is common in cases of rectal prolapse. - Fecal Incontinence:
Difficulty controlling bowel movements, leading to leakage of stool, can occur in more severe cases. - Feeling of Incomplete Evacuation:
A sensation that the bowel hasn’t been fully emptied after a bowel movement.
If you’re experiencing any of these symptoms, it’s essential to seek medical attention promptly. Early diagnosis and treatment can prevent complications and improve outcomes.
Diagnosis of Rectal Prolapse
At Rai Piles Health Clinic, Dr. Yogendra Rai uses a combination of clinical evaluation and advanced diagnostic tools to accurately diagnose rectal prolapse. The diagnostic process typically includes:
- Medical History:
A detailed discussion of your symptoms, diet, lifestyle, and medical history. - Physical Examination:
A thorough examination of the anal and rectal areas to check for protrusion, swelling, or other abnormalities. - Digital Rectal Exam (DRE):
The doctor inserts a gloved, lubricated finger into the rectum to feel for any abnormalities. - Defecography:
This imaging test involves taking X-rays or MRI images while the patient defecates to visualize the rectum and pelvic floor muscles. - Anorectal Manometry:
This test measures the muscle strength and coordination in the rectum and anus. - Colonoscopy:
In some cases, a colonoscopy may be recommended to rule out other conditions like colorectal cancer or inflammatory bowel disease.
Treatment Options for Rectal Prolapse
The treatment of rectal prolapse depends on its severity, the patient’s overall health, and the presence of any underlying conditions. At Rai Piles Health Clinic, Dr. Yogendra Rai offers a range of treatment options tailored to each patient’s unique needs. Here are some of the most common approaches:
- Lifestyle Modifications
For mild cases of rectal prolapse, lifestyle changes can often provide relief. These include:
- High-Fiber Diet:
Eating more fruits, vegetables, whole grains, and legumes can help soften stools and reduce straining during bowel movements. - Hydration:
Drinking plenty of water throughout the day can prevent dehydration and soften stools. - Pelvic Floor Exercises:
Strengthening the pelvic floor muscles through exercises like Kegels can help support the rectum and prevent prolapse. - Avoiding Straining:
Avoiding heavy lifting and straining during bowel movements can reduce the risk of further prolapse.
- Medications
In some cases, medications may be prescribed to help manage symptoms and promote healing. These include:
- Stool Softeners:
Medications like docusate sodium (Colace) can help soften hard stools. - Laxatives:
Bulk-forming laxatives like psyllium (Metamucil) can help regulate bowel movements. - Pain Relievers:
Over-the-counter pain relievers like ibuprofen or acetaminophen can help manage discomfort.
- Non-Surgical Procedures
For some patients, non-surgical procedures may be recommended. These include:
- Pessary:
A pessary is a device inserted into the vagina to support the pelvic organs and reduce prolapse symptoms. - Sclerotherapy:
Injecting a sclerosing agent into the rectal tissue can help shrink the prolapsed tissue.
- Surgical Options
For more severe or chronic cases of rectal prolapse, surgery may be necessary. The most common surgical procedures include:
- Rectopexy:
This procedure involves securing the rectum to the sacrum (the lower part of the spine) using sutures or mesh to prevent it from prolapsing. - Resection Rectopexy:
In this procedure, a portion of the rectum is removed, and the remaining rectum is secured to the sacrum. - Perineal Procedures:
These procedures, such as the Altemeier or Delorme procedures, involve removing the prolapsed rectum through the anus and are often used for patients who are not candidates for abdominal surgery.
Recovery and Aftercare
Recovery from rectal prolapse treatment varies depending on the procedure performed. Most patients can expect some discomfort and swelling for a few days after treatment. At Rai Piles Health Clinic, we provide detailed aftercare instructions to ensure a smooth recovery, including:
- Keeping the area clean and dry.
- Taking prescribed medications to manage pain and prevent infection.
- Avoiding strenuous activities until cleared by your doctor.
- Following a high-fiber diet to prevent constipation and strain during bowel movements.
Why Choose Rai Piles Health Clinic?
At Rai Piles Health Clinic, we specialize in the diagnosis and treatment of rectal prolapse and other anorectal conditions. Here’s why patients trust us:
- Expertise: Dr. Yogendra Rai and his team are highly skilled in the latest diagnostic and treatment techniques.
- Personalized Care: We tailor our treatment plans to meet the unique needs of each patient.
- Advanced Technology: We use state-of-the-art equipment to ensure accurate diagnosis and effective treatment.
- Compassionate Approach: We understand the sensitive nature of anorectal conditions and provide discreet, empathetic care.
Prevention Tips
Preventing rectal prolapse is often easier than treating it. Here are some tips to help keep your digestive system healthy and reduce the risk of prolapse:
- Eat a Balanced Diet:
Include plenty of fiber-rich foods in your diet to prevent constipation. - Stay Hydrated:
Drink at least 8 glasses of water a day to keep stools soft. - Exercise Regularly:
Aim for at least 30 minutes of physical activity most days of the week to promote regular bowel movements. - Practice Good Bowel Habits:
Avoid straining during bowel movements and respond to the urge to go promptly. - Strengthen Pelvic Floor Muscles:
Regular pelvic floor exercises can help support the rectum and prevent prolapse.
Conclusion
Rectal prolapse can be a painful and distressing condition, but with the right treatment, it can be effectively managed. At Rai Piles Health Clinic, Dr. Yogendra Rai and his team are committed to providing the highest standard of care to help you manage and overcome rectal prolapse. If you’re experiencing symptoms of rectal prolapse or have been struggling with this condition, don’t hesitate to reach out to us. Our team is here to guide you every step of the way.
For more information or to schedule a consultation, visit our website or contact Rai Piles Health Clinic today. Your health is our priority.